What can be done to relieve my symptoms?
Physiotherapy can be very effective at easing your current pain and getting you back to your normal everyday activities. This is because physiotherapy has proven to be beneficial for both acute and chronic back pain. Furthermore, physiotherapy can assist patients of all ages and at all stages of back pain, whether this is your first bout of pain, or you have had several bouts and are now experiencing chronic pain. In addition, physiotherapy can help by educating you about how to prevent back pain flare-ups in the future.
Although the time required for rehabilitation varies among patients, you should expect to participate in therapy for anywhere from three weeks to four months, depending on whether your problem is acute or is a chronic issue. The recommended treatment will also depend on how painful and debilitating your back pain is.
Even though back pain can be scary and physically restricting, it is very rarely a sign of serious tissue damage or a dangerous underlying condition. In the majority of cases, back pain responds very well to physiotherapy treatment. Each of our treatment approaches are designed specifically for your individual type of back pain. Furthermore, the main goals include working toward easing your pain, improving your mobility, strength, and posture, and enhancing back function. In addition, your physiotherapist at Next Step Physio will teach you how to control your symptoms and how to protect your spine for many years ahead.
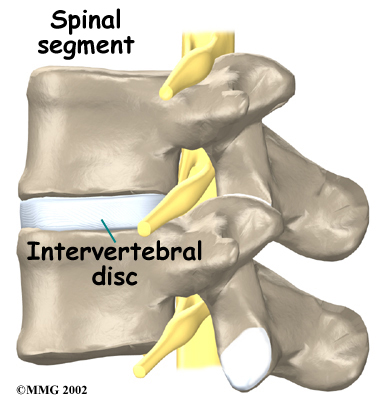
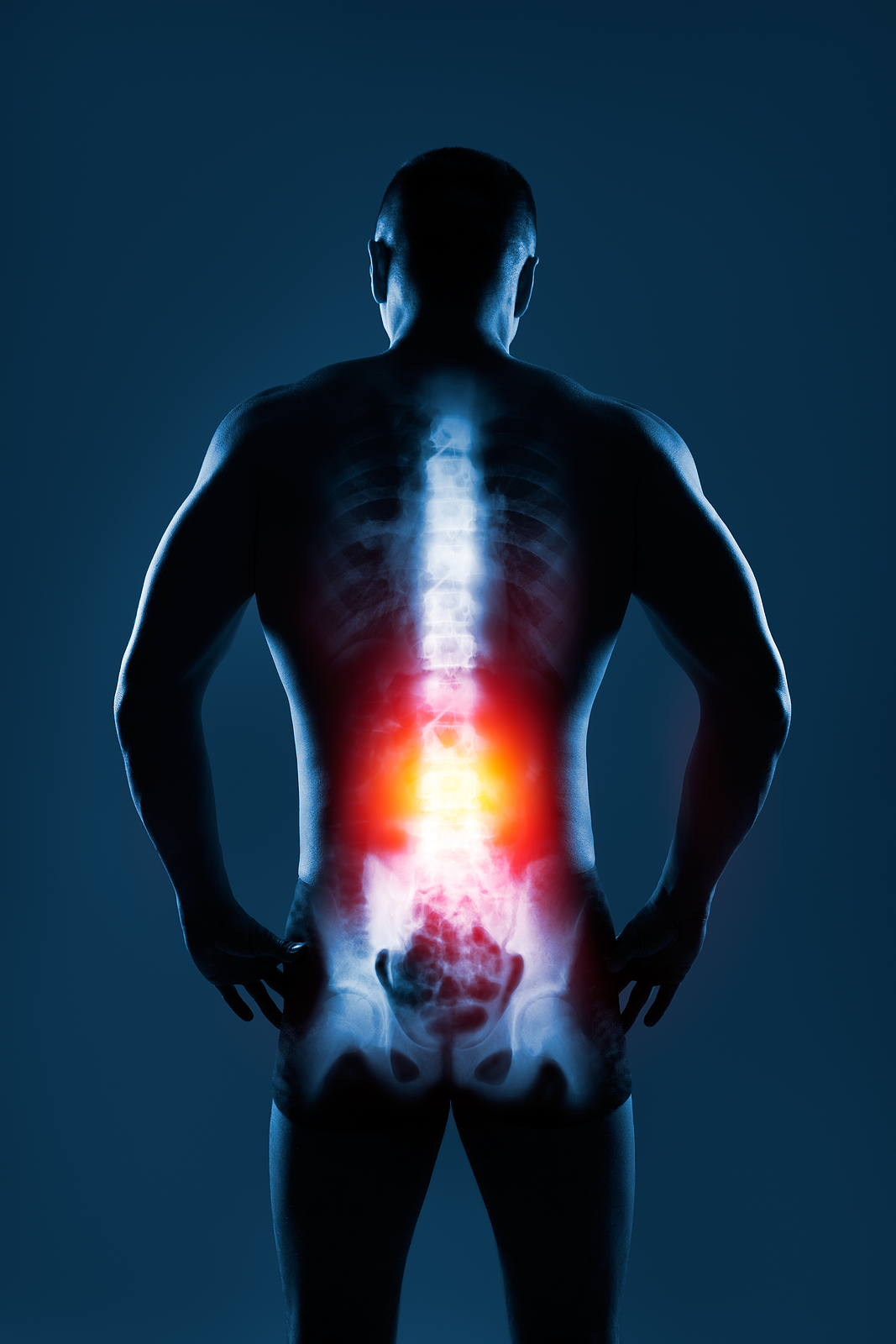
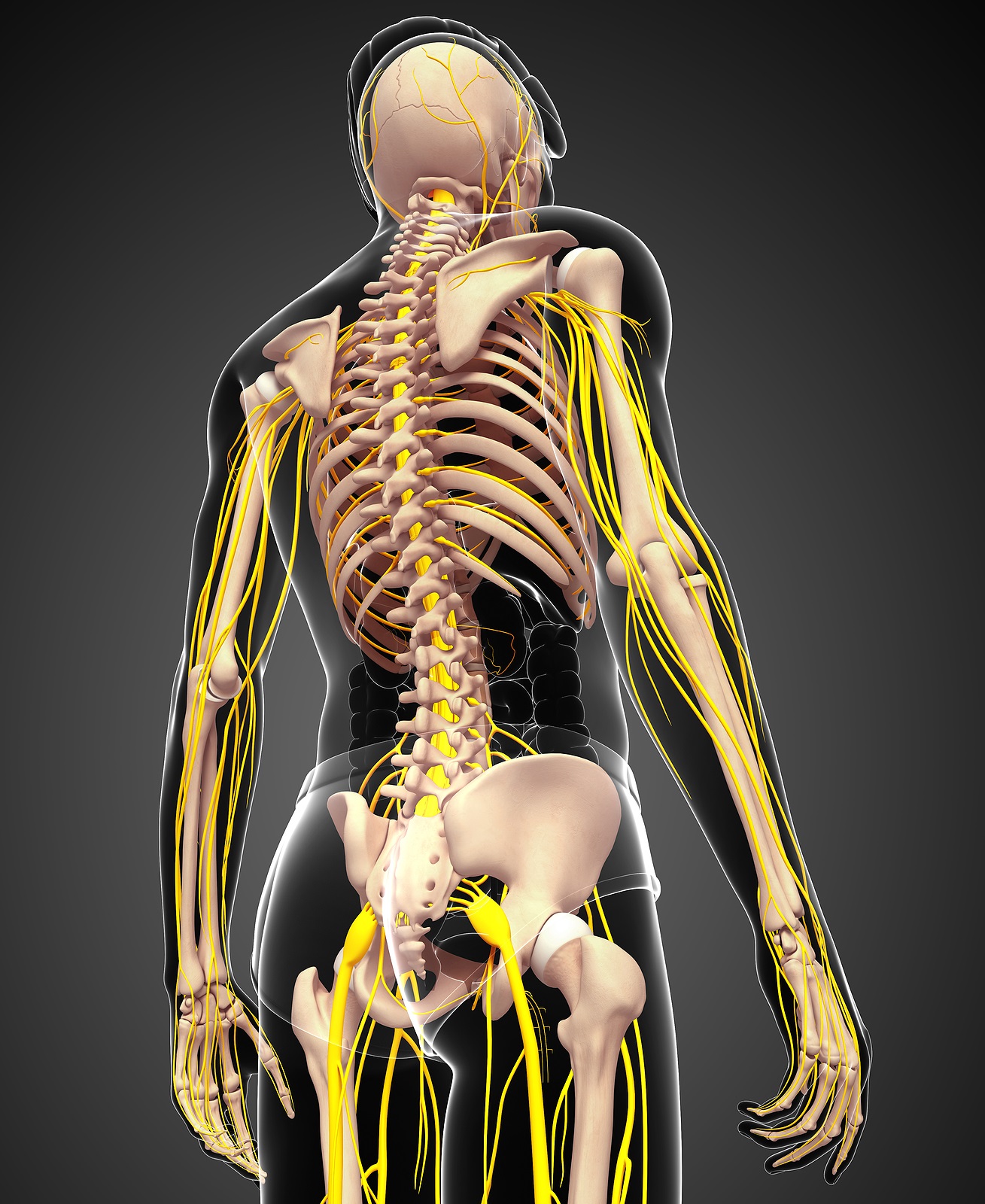
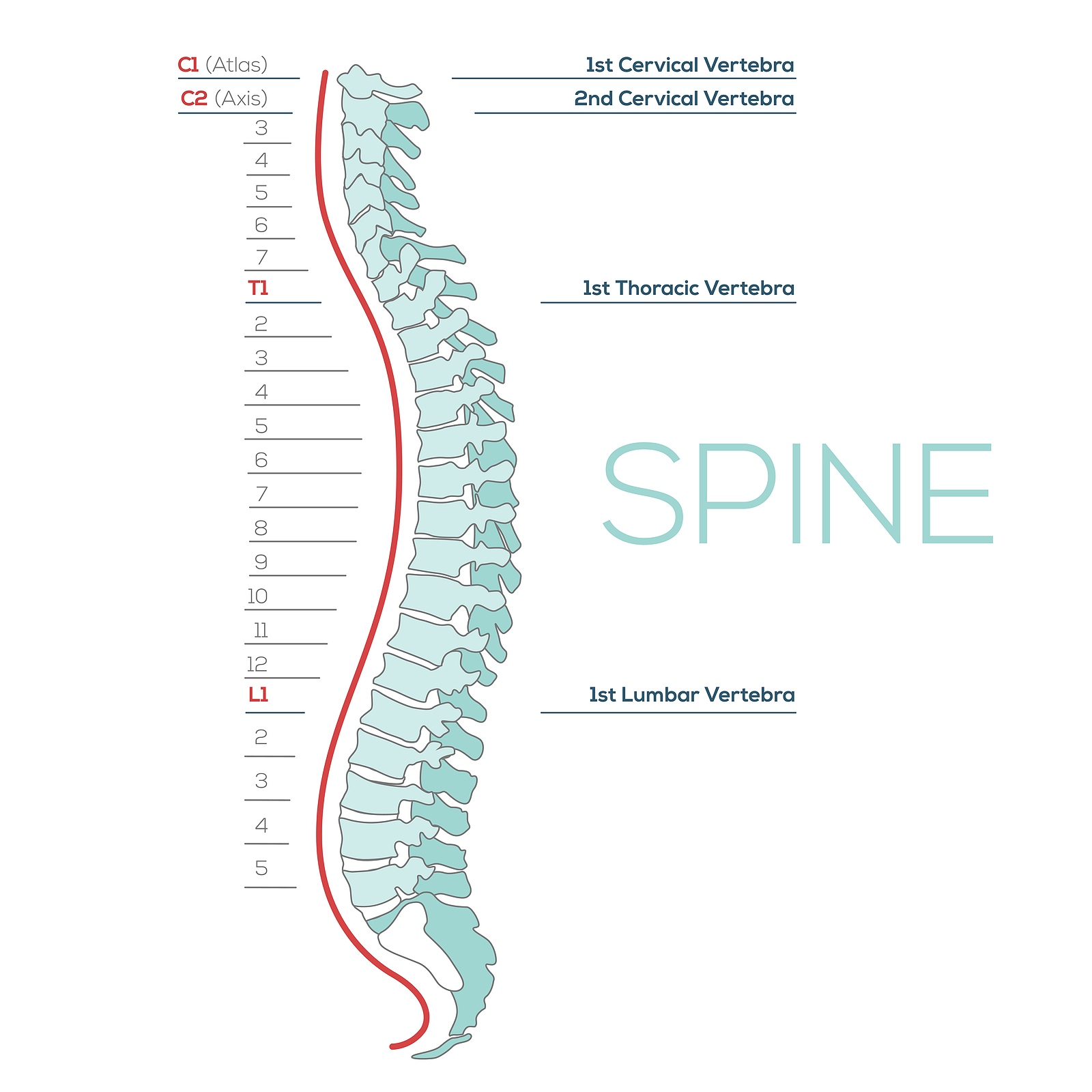
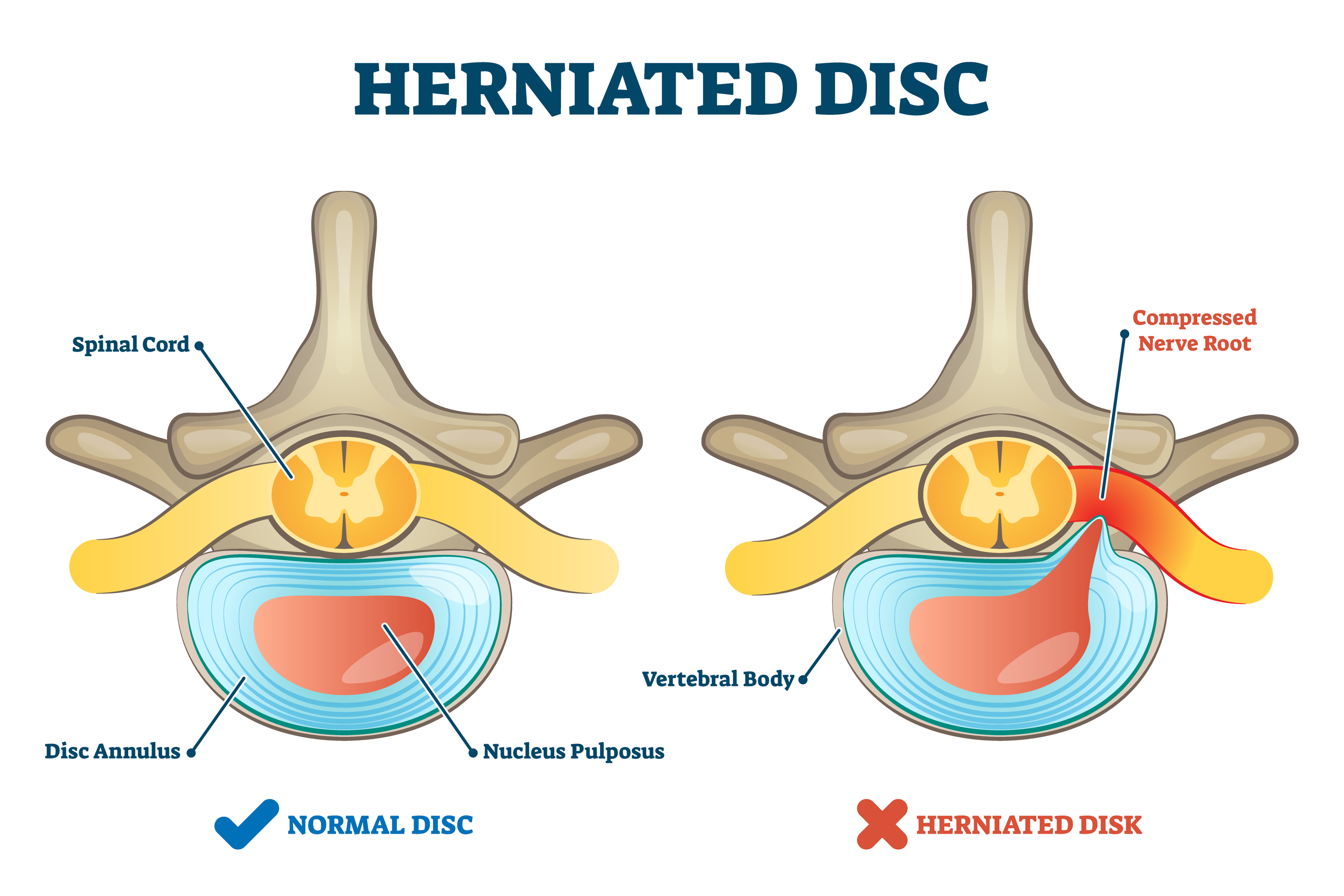
If your low back pain is an acute flare-up of less than 2-3 weeks, your physiotherapist may initially use ice, heat, ultrasound, electric muscle stimulation, interferential current, laser, needling (acupuncture), or hands-on treatment to address your symptoms. These modalities may be particularly helpful during the early weeks to improve your comfort so you can more easily. Adhering to your physiotherapy regimen is an optimal way to quickly get back to your normal activities. Pain education will also be an important aspect of your therapy right from the start, as it can help you understand the nature of your low back pain. In addition, understanding the anatomy of the back and factors that contribute to back pain can help address your fears or beliefs about back pain. Furthermore, engaging in physiotherapy can reduce apprehensions regarding your prognosis, help improve self-empowerment, and decrease the likelihood of developing chronic pain.
Your physiotherapist will also teach you ways to position your spine for maximum comfort while you recover from your injury or flare-up. Your back is designed to withstand a variety of postures and it is healthy for your back to frequently move into many different postures. As long as you are without pain at the time, slouched sitting as well as lifting items with a slightly rounded back are okay for your back! The anatomical structures that support your spine can still work efficiently in these postures. You and your physiotherapist may explore your preferred directions of movement and how to use them to your advantage as you heal. As rehabilitation progresses, it will be very important to explore and practice all directions of movement, and your therapist will guide your individual journey to movement freedom. Your physiotherapist will also explore efficient sitting, standing, and movement postures as well as techniques that help you rediscover the strength and resilience of your spine.
At times, you may be tempted to stop all activity because of your low back pain. It is important to avoid inactivity, as there is a great deal of evidence that shows how beneficial aerobic exercise such as walking, running, or biking helps in the treatment of low back pain. Increased overall fitness also reduces the risk of developing back pain again. Furthermore, moderate to severe pain during activity should always be addressed, but mild discomfort may occur as you start to resume your activities and as your back recovers. Minor discomfort that lingers as you return to daily activities does not mean you are further injuring structures in your back. Intense activity may need to be discontinued temporarily, but gradually returning to your regular routine will be good for your back and your overall health in the long run. Your physiotherapist can help you determine the best activities to start with and the most appropriate way to perform them with your particular injury. The physiotherapist can also assist you in deciding how hard you should push your activity level at each stage of your rehabilitation.
In addition to getting back to regular aerobic exercise, your physiotherapist will teach you specific strengthening and stretching exercises to help your back. Your hip range of motion and strength is particularly important in helping your back function properly, so the physiotherapist will assess your hips and lower body alignment to demonstrate the ideal strength and mobility exercises for your individual needs. These types of exercises address tightness, weaknesses, and side-to-side imbalances.
Your ‘core’ muscles are located around your abdomen and trunk. They help maintain flexible (not rigid) stability in this area. These muscles also ensure efficient load transfer to the lower back and the entire spine. Maintaining adequate core strength is important for anyone, but particularly for those with low back pain. Some patients with chronic back pain unintentionally ‘overuse’ or inappropriately use their core muscles, and this can be more detrimental to someone with back pain than an individual who is not regularly active. Your physiotherapist will check your core activation and strength to teach you how to appropriately and efficiently use your core muscles to support your spine during daily activities. A key aspect of therapy will be teaching you how to move without holding your breath to allow you to engage these muscles efficiently and with less pain. Remember that your back is anatomically designed to withstand the loads of everyday life such as bending, twisting, jumping, and lifting heavy objects. Your physiotherapist will educate you on proper postural movements to ensure you are taking the right steps to optimize your back’s abilities.
If you have severe back pain, the physiotherapist may choose to work with you in a pool or encourage you to do exercises in a pool on your own. Physiotherapy performed in water puts less stress on your low back, and the buoyancy allows you to move more easily during exercise. Clients consistently report how much easier it feels to move their back when they are in the water.
It is well known that other factors can drastically affect your chances of getting low back pain and also how quickly you heal from your discomfort. As mentioned previously, people who smoke have both a higher risk of experiencing low back pain and recovering from it more slowly, as smoking decreases the blood supply to tissues and bones. Decreased blood flow leaves tissue vulnerable to injury, accelerates degeneration, and delays healing. Your physiotherapist will encourage you to stop smoking if you currently smoke. Even temporarily quitting while you are addressing your back pain helps, but quitting for good is highly recommended.
Apprehensions, emotions, and personal beliefs also heavily influence the experience of back pain and the recovery trajectory. If you believe your back is unstable, fragile, or undergoing degenerative changes, it will be hard to trust that guided movement is safe. Furthermore, if someone in your family has lived with horrible back pain, you may be inclined to believe that this is also your fate. This is another factor that can influence your experience. In addition, if you have experienced back pain and recovered from it, you may feel similar sensations and discomfort again if you experience emotional trauma, loss, or anxiety. Your physiotherapist is aware of these factors and may perform additional assessments to determine if your pain is being created by the brain, rather than in response to tissue damage. In either case, your physiotherapist knows the pain you experience is real and that you are not suffering from intangible pain. Treatment approaches for centralized (or nociplastic) pain may be targeted at restoring your sense of safety, exploring your beliefs about your back pain in a non-judgemental way, and possibly getting you additional support to help process the emotional strain.
Being overweight can also affect your lower back, particularly if you carry your weight around your abdomen. This indicates a higher body fat percentage and therefore higher systemic inflammation. If appropriate, your physiotherapist will encourage you to lose weight and modify your eating, sleep, and exercise patterns, which will help you recover more quickly and avoid future flare-ups.
Physiotherapy at Next Step Physio will focus on reassuring you that swiftly getting back to work and other normal activities won't cause you harm and can actually help improve your back’s tolerance for activity in the future. Nonetheless, back injury flare-ups may occur in the future and are often related to a period of emotional trauma, low mood, poor mental health, disrupted sleep, stress, inactivity, or trying a new activity. Your physiotherapist will discuss what steps to take if your back pain returns.
Your physiotherapist can also show you how to keep moving with efficiency during routine activities. You'll learn about healthy postures for your back and using the best body mechanics to assist your back while lifting and carrying, standing and walking, and performing work duties. The anatomical structure of the back naturally accommodates activities such as carrying heavy loads, as well as sitting and standing for periods of time. Contrary to popular belief, a slouched sitting position and allowing your back to bend forward slightly while lifting items is actually conducive to how your back is designed and is considered proper body mechanics! These positions allow the layers of long and tough ligaments and muscles at the back of the spine to do their job in supporting the spine. In addition, our bodies are made to move instead of staying in one position for too long, especially when recovering from injury. Your physiotherapist can guide your movements as you recover from your back pain.
Bed Rest
Although ‘bed rest’ was a common prescription in the past for acute back pain, ‘bed rest’ or lying down and remaining stationary is rarely prescribed to help back pain these days. Alternatively, in cases of severe pain, your physiotherapist may suggest a short period of ‘modified rest’ where you are encouraged to rest in a comfortable position, such as on your back with your knees supported or in a semi-reclined position in a chair. Modified rest permits moderate activities, such as gentle hip and back exercises within the normal range of motion or light walking to keep your back moving while allowing your acute pain to settle. Staying in one position for too long, although it may feel comfortable at the time, is actually detrimental to healing. For this reason, modified rest after an acute injury will only be recommended for no more than 2-3 days.
Back Braces
A back support belt is sometimes recommended when back pain first strikes. In many cases, a back brace can help provide support by adding compression to your back and increasing your confidence when you move. A brace can also lower the pressure inside a problem disc, decrease pain, and allow you to engage in some activities longer than you could without the back brace. Your physiotherapist will gradually encourage you to discontinue wearing the brace as your pain improves and you can engage in more advanced back strengthening exercises. Using the brace routinely after recovering from acute pain is not recommended. Wearing a back brace all the time after your back has recovered may cause muscles to atrophy (shrink) and some patients will psychologically begin to rely on the belt instead of on the strength of their own muscles.
Medications
Your physiotherapist will suggest that you consult with your doctor or pharmacist regarding the use of pain relief or anti-inflammatory medication for your acute back pain. Although there is no medication that will cure low back pain, short-term medications that combat pain, inflammation, and muscle spasms may be useful supplements for your rehabilitation program. Over-the-counter medication is sufficient for most cases of back pain and helps support restful sleep. Persistent back pain is often linked to sleep problems.
Next Step Physio provides services for physiotherapy in Edmonton.